Contemplative Care & Spirituality:
Going Beyond Mindfulness Practice for Being with Suffering & Grief
Introduction
The practice of Buddhist based mindfulness meditation is now sweeping the
world. Entering various secular fields like business, medicine, and even sports,
mindfulness practice has helped people to reduce work related stress, be more
efficient and focused in their endeavors, and find a pathway to inner peace.
There are, however, critics of this movement-including the Buddhists that
helped spawn it-who point out that mindfulness meditation (samadhi) in and
of itself is not sufficient for true transformation and that isolating it
from the ethics (sila) and a deeper understanding of the roots of ignorance
(panna) can distort the practice in unfortunate ways. Furthermore, as wonderfully
simple as mindfulness may seem, it is usually not a practice that is accessible
for the deeply traumatized, such as those experiencing suicidal depression,
recovering from a natural disaster or traumatic event, or dealing with the
grief of a lost loved one. To become intimate with such people, and to be
able to guide them to a place of stability from which an intensive mindfulness
practice could be of help, requires a type of caregiver or "guide"
who is in fact highly developed in all three of these facets of mindfulness,
ethics, and the accompanying wisdom and resilience it requires to engage deeply
in suffering.
On November 4, 2017, these two issues-understanding mindfulness in a more
holistic manner and applying this holistic approach to caregiving-were grappled
with at a public symposium jointly hosted by the Rinbutsuken Institute for
Engaged Buddhism, the Catholic based Sophia University Institute of Grief
Care, and the Tokyo Jikei Medical University Palliative Care Center. Both
the Rinbutsuken Institute and the Sophia Grief Care Institute are organizations
within Japan that have recently started cultivating such caregiver guides,
which in the professional world are often called "chaplains". Working
from different religious standpoints but in cooperative settings, these two
organizations are confronting the various forms of suffering now prevalent
in Japan, such as depression, suicide, disaster trauma, the death of so many
elderly, and all the grief that accompanies these issues.
While the Rinbutsuken Institute and the Sophia Grief Care Institute have been
collaborating across religious lines for a few years, this symposium was a
landmark event in the collaboration between medical and religious worlds in
Japan. The modern medical world has largely dismissed the role of religious
professionals in the care of patients, although the practice of "team
care" with certified, professional chaplains has become somewhat standard
in the United States. Since the end of World War II, Japan has been a resolutely
secular state and has constitutionally barred the role of religious professionals
in public sector work. This symposium was the first time a top level medical
school, such as the Jikei School of Medicine, has collaborated with religious
based organizations for a public event on the ways to collaborate for better
patient care.
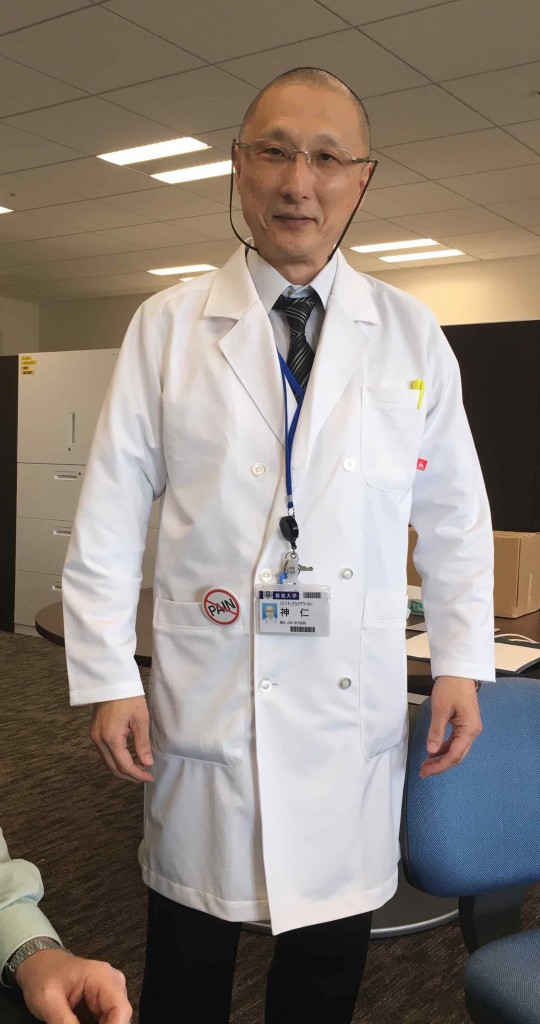
The host of the symposium was Prof. Dr. Naohito Shimoyama, Head of the Department
of Palliative Medicine at Tokyo Jikei Medical University. Along with his wife
and co-collaborator, Prof. Dr. Emi Shimoyama, they have recently brought in
the Director of the Rinbutsuken Institute, Rev. Hitoshi Jin, and his colleague,
Rev. Gakugen Yoshimizu, to serve as spiritual care workers and Buddhist chaplains
at the hospital. A third collaborative partner was Prof. Susumu Shimazono,
who was a leading scholar on contemporary religion at Tokyo University and
is now the Director of Sophia's Grief Care Institute while also serving on
the Board of Directors for Rinbutsuken. These collaborative connections across
independent organizations were until recently extremely difficult to cultivate
in Japan, but are now breaking new ground for the future of holistic care,
both medical and spiritual.
Presentations on Going Beyond Mindfulness Practice for Being with Suffering
& Grief
To galvanize such collaboration, the Rinbutusken Institute with its international
networks brought in three caregiver guides or "chaplains" from different
parts of the world for this one-day symposium: Prof. Elaine Yuen, Associate
Professor and Chair of the Department of Wisdom Traditions at Naropa University
in the United States; Rev. Gustav Ericsson, a Christian priest in the Lutheran
Church of Sweden with Japanese Soto Zen ordination; and Ven. Kuppiyawatte
Bodhananda Thero, the founder and the Director of the Mithuru Mithuro Movement,
the first and the largest Buddhist drug rehabilitation center in Sri Lanka.
These three speakers are all using a range of contemplative practices that
include mindfulness to be with the suffering of the traumatized. However,
they brought to the audience a much wider understanding of mindfulness as
not just a breathing technique for stress reduction but also as a method which
combined with other forms of spirituality can develop numerous pro-social
qualities for caring for others and transforming institutions.
Prof. Yuen began the symposium by immediately introducing a different seminal
concept in Buddhism than mindfulness, that is compassion (karuna). She noted
that healthcare is by nature centered around interpersonal connection, because
at its root an awareness of and feeling for the pain and suffering of others
impels and empowers people to not only acknowledge but also act. This is the
essence of compassion. However, in such intensive environments like hospitals
where there is so much suffering, something called "compassion fatigue"
often occurs. This is a stress response from caring without expected rewards,
results, and often closure that results in a diminished capacity for empathy
and interpersonal engagement. Such "compassion fatigue" manifests
in a variety of issues for caregivers, such as burnout from cumulative work,
demands, and stress; secondary trauma from the dysfunction that arises from
prolonged exposure to the suffering of others; moral distress from conflicts
when a clinician knows what is right but cannot do it; horizontal hostility
from disrespect among members of their professional peer group; and the structural
violence inherent in many modern medical institutions which amongst other
things must balance profit with care.

To meet these problems, she explained, mindfulness practice for the caregiver has become an increasingly important and popular practice in the United States. This shift has occurred from the mounting research evidence of its effects on emotional regulation and improved attention, greater calm and stress reduction, and enhanced coping skills. However, Prof. Yuen and other Buddhists in the field are now trying to integrate other Buddhist based contemplative strategies, such as "self-compassion". Drawing on a variety of Buddhist teachings-especially the Four Divine Abodes (brahma-vihara) of loving-kindness (metta), compassion (karuna), sympathetic joy (mudita), and equanimity (upekkha)-American Buddhists in clinical and hospital environments are attempting to practice and transmit practices to develop warmth and understanding in oneself in times of professional suffering, failing, and feeling inadequate. Prof. Yuen explained that this involves practices to develop?empathy and the ability to regulate one's own arousal to situations so that one develops resilience rather than becoming overwhelmed. There is also the practice of perspective taking to develop congruence in goals and values between fellow clinicians and patients and their families. The practice of moral sensitivity is another important key in being able to recognize conflicts and obligations within the institution and to support caregiver decision-making. In this way, Prof. Yuen outlined the ways the holistic Buddhist approach of ethics (sila), meditation (samadhi), and causal insight (panna) work together to support a caregiver in navigating the wide variety of issues that arise in working in healthcare organizations.
Ven. Bodhananda from Sri Lanka took the audience into a deeper understanding this key practice of the Four Divine Abodes, which are so critical in developing the skills that Prof. Yuen discussed. Ven. Bhodhananda's work has not been in the kinds of public healthcare facilities that Prof Yuen outlined but in his own drug rehabilitation center for young men that he established in 1987. The name of the organization, Mithuru Mithuro, means "compassionate friend", and the unique aspect of his center is the creation of a family system rather than a professionalized institution. All senior staff and counselors at the center were former patients themselves, creating a shared intimacy and respect among first time addicts and fully rehabilitated elder brothers. In explaining the process of their center, Ven. Bodhananda noted that if one is willing to work with suffering in order to help others to relieve their pain, first they must strengthen their own personalities by developing the basic human qualities according to the Buddha's teachings of loving-kindness, compassion, sympathetic joy, and equanimity. He explained that these practices help to level social barriers, build harmonious communities, revive joy and hope long abandoned, and promote human brotherhood against the forces of egotism. In a therapeutic community, he has found these are very important to enhance treatment.

Ven. Bodhanana then explained the actual practice of meditation on these four "sublime states", a practice that is as common in world of orthodox Buddhism as is basic mindfulness practice. For an example, he explained, we might select loving kindness as the specific subject of meditation. First, we start with an aspiration for our own wellbeing, using it as a point of reference. Then we gradually extend it to other beings by starting with someone we have loving respect for, like our parents or a teacher, then to dearly beloved people, to indifferent ones, and finally to enemies, if any, or those disliked. Persistent meditative practice of this method, he explained, will make these four qualities sink deep into the heart so that they become spontaneous attitudes. This practice will systematically break down conflicts we have with others, and we will be able to be more sensitive towards their suffering.
Ven. Bodhananda concluded by saying that the rehabilitation process followed by Mithuru Mithuro is not only for drug addicts. Anyone is who is suffering, as well as caregivers who are expected to offer support, can follow this process in order to develop these sublime states in themselves. He emphasized that we cannot categorize the distressed into a permanent group, because we all have the tendency to face similar addictions in our lives. We all are in same boat, so all are subject to addiction if we are not developing our spirituality. In this way, Ven. Bodhananda's vision is not limited to using mindfulness and other Buddhist practices to develop coping mechanisms but is rather much vaster to include the fundamental transformation of each individual. Having rehabilitated over 5,000 addicts since 1987, Ven. Bodhananda center has been transforming young men into true leaders in society, who have been able to go forth and offer guidance and support to others in sorrow or fear, in stress or trauma.
Rev. Gustav Ericsson also brought a deeper and more nuanced understanding of meditative mindfulness in his talk. Before becoming a priest in the Lutheran Church of Sweden in 2010, Rev. Ericsson began his spiritual journey studying and practicing Japanese Zen in mid 1990's and then receiving Dharma transmission from the Soto Zen teacher Gudo Nishijima Roshi in 2004. After being ordained as a Christian priest, he has served as a hospital chaplain at the regional University Hospital of Umea in northern Sweden and at a hospice for palliative care. He has also served as a counseling priest with the Lutheran Church's national suicide prevention hotline, which has a national emergency number as well as chat rooms and mailbox online.
Rev. Ericsson explained that the key principles of his chaplaincy-being aware of his inner prayer room, walking slowly, entering a room with empty hands, seeing the Christ that is already here, and releasing the weight-are all to a large extent upheld and nourished by his practice of sitting and walking meditation. He noted that the sitting and walking of Zen meditation has become one with his service as a Christian hospital priest. He then explained how Buddhist mindfulness training has served as a platform for incorporating a variety of deeper practices. When he started working at the hospital, one of the first things his religious colleagues invited him to do was to practice embodying himself as a prayer room. For him, this is an image of how to be present in hospital rooms, corridors, and wards as a sitting and walking prayer room, which means providing an open and welcoming space that has many possibilities.
Another important practice for Rev. Ericsson is to enter every room with empty hands. This means letting go of ambitions and ideas about what to say, do, and accomplish. Rev. Ericsson explained that he tries to empty himself in order to be able to receive the people and the situation that he meets in the room and to enter with open questions and a willingness to listen and learn how he can be of service. For him, this practice of entering a room with empty hands does not mean that he denies his training, experience, and knowledge. Rather, he noted that in the moment of touching the handle and opening the door, he practices letting go of ambitions, tools, and fixed ideas while trusting in something bigger than his own thoughts and something greater than his little self. Rev. Ericsson insights here-the emptying of the self so that one can be "enlightened" by others forms -embody the essential Buddhist wisdom (panna) that comes about from a deeper meditative insight (vipassana) attained beyond the basic calming and de-stressing (shamatha) of mindfulness practice.

Panel Discussion and Conclusion
After the conclusion of these presentations, Dr. Shimoyama, Rev. Jin, and
Prof. Takaki Ito offered some short comments and then questions which led
to a wide ranging two hour discussion. One of the most important issues that
arose was the continued struggle to harmonize and coordinate the disparate
approaches towards care of the medical and religious worlds. Prof. Ito of
the Graduate School of Applied Religious Studies at Sophia University noted
that the medical model focuses on objectivity and rationality in a diagnostic
analysis. However, today's speakers did not speak of a linear cause and effect
model, but more of a dialectical model involving an interaction or relationship
between patient and caregiver that includes subjective modalities like hope,
the meaning of life, and values. While Prof. Ito said that he is sympathetic
to these approaches, he noted that in Japan, as opposed to many other countries,
there is absolutely no dialogue around spiritual or contemplative care in
the medical world. In this way, he feels the need for some sort of data or
evidence of these spiritual care methods to gain a foothold in Japanese medical
institutions to be able to begin this work.
Prof Yuen responded that in the United States there is increasing research
on the impact of chaplaincy, especially in terms of the financial bottom line
of hospitals and their need to save/make money and to increase consumer satisfaction.
Rev. Jin and his colleague at Rinbutsuken, Jonathan Watts, learned about this
work on their visit to John's Hopkins Hospital, which has a number of quantitative
research studies on the effects of chaplaincy services. Rev. Ericsson noted
that his hospital in Sweden developed a customer satisfaction survey with
about 50% of positive results coming from how patients and family were received
and handled, a role in which chaplains can be an important part. Prof. Yuen
cautioned, however, that the work of the chaplain and their positive effect
is often in special encounters when a meaningful contact or communication
is made, like a sacred moment. This is very hard to do a quantitative analysis
of and develop a predictive model for, even though its effect is well understood.
Rev. Ericsson concurred that it is clear that there are special spiritual
moments for the dying and their families, but that it is problematic to try
to measure, quantify, or pre-arrange.
In response to this extended dialogue, Dr. Shimoyama provided the closing
remarks for this groundbreaking symposium. He admitted that medical people
have been very resistant to the religious world, but added that there is much
in medicine and palliative care that cannot be explained by science. He reflected
that sometimes when he is with a patient, he just wants to run away because
the suffering is so severe. There are problems like this that cannot be solved
by science, and religious people can help fill in these gaps. Thankfully,
he was made aware of these issues by the late Dr./Rev. Masahiro Tanaka-a graduate
of Jikei University and a Shingon Buddhist priest who ran a hospital and care
home from his own temple in Tochigi. Rev. Tanaka's temple has served as a
training center for chaplains-in-training from the Rinbutsuken Institute,
and it was Rev. Tanaka who introduced Rev. Jin to Dr. Shimoyama and Jikei
University Hospital. Dr. Shimoyama concluded that he now feels very proud
to be working with religious people. The important thing is to realize what
we are lacking and to aim higher. We cannot accomplish much on our own, but
when we join together with others, we can achieve greater results. In this
way, he hopes Jikei University can become a center for the advancement of
this work. Re-iterating Prof. Shimazono's final comments for greater cooperative
work, the symposium closed with the feeling that a new beginning had taken
place in Japan for the interface of medical and spiritual as well as contemplative
care for "all beings in this world of suffering".

This report was prepared by Jonathan Watts, Research Fellow at the Rinbutsuken Institute, Lecturer at the Sophia University Grief Care Institute, and Executive Board Member of the International Network of Engaged Buddhists (INEB).
Watts: one thing that is measureable is customer satisfaction and whether
or not that increases with a chaplain on call. Hopkins is doing this research
Yuen: She studied with JKZ about levels of stress and see how that correlates
to well being and spiritual care.
Taisho Dai Korean Nun: what's the biggest thing to get from meditation? How
to support people in crisis beyond saying Ganbatte?
Gustav: Zazen helped me at first to disconnect from his conceptual word based
mind. But further it has helped him feel closer to others and reality. With
impossible or difficult situation, just breathe together and to be together
and say I am here for you.
Yuen: When she met Trungpa, she felt she was able to recognize some aspect
of her mind and sense of clarity and self-recognition of that clarity so meditation
helps her reconnect with that. For people in crisis, not so much asking questions
but being present and trying to notice what around them they have collected
helps them to open up and is life affirming and help them to touch that.
Jochi Dai Student:
Yuen:
Jin: we need three kinds of connection to live our lives well: 1) ourselves
2) family 3) something greater than the self (nature, God etc.) We greet the
buddha nature in each person when we encounter them so we don't need to save
them but rather help them awaken to it.
Hospital Nurse: How to practice Brahmaviharas with patients when you don't
feel it?
Bodhananda: whenever a problem arises or you feel bad, recollect those four
states and you will begin to feel better but it takes time and eventually
you get results.
Gustav: I might take a bathroom break where I re-collect myself and then later
talk to a colleague for support. These difficult feelings are part of the
practice. We're not failing but we're actually engaging.
Shimazono: I would like to increase our connections and meeting and sharing
because you three speakers have so much experience that we can learn from.
I would also like to know what you three think of the Japanese situation?
Bhodhananda: Much to learn from Japanese Buddhism to improve ourselves
Yuen: First time in Japan for me. Some similarities between Japan and US in
emphasis on science in medicine and now an opening to chaplaincy. As opposed
to U.S., Japan has deep tradition and that might actually be a barrier to
entering into the modern era and making it accessible for modern people and
having them be interested in it. His mom became Christian growing up in China
because it was new and accessible. What's that spark that attracts people
before institutionalization sets it. So I encourage you to keep exploring
and asking questions.
Gustav: Prof. Ito's question about measurements is important and how to continue
to try to develop these approaches. Hitosaji message of one spoonful is meaningful,
what we can do now, little by little.
Jin: Kanehiro Takagi passed away in 1920. Year of Tokyo Olympics will be
his centennial. I'd like to reflect on the founding spirit of this hospital.
Prof. Ito: For a university hospital to have such a symposium is possibly
epoch making. We have a history of Christian chaplains in Japan but we need
chaplains in public spaces so this symposium today is very important and the
efforts of Jikei are every important.
Dr. Shimoyama: We are doing cutting edge research on palliative care here.
There was a time when medical people were resistant to religious world. There
is a lot in medicine and palliative care that can't be explained by science.
Sometimes when I am with a patient I want to run away because the suffering
is so severe. Dr/Rev Masahiro Tanaka helped to connect me to rev Join and
make us aware of what we have been lacking. We have always valued science
but the medicine is not limited to science. There are problems that can't
be solved by science and religious people can help fill in these gaps. I feel
very proud to be working with religious people. The important thing is to
realize what we are lacking and to aim higher. We often can't do things on
our own but when we join together with others we can achieve greater results.
Dr. Ito has also joined us as a colleague here. We hope Jikei University can
become a center for the advancement of this work
Two Hour Panel Discussion
JIN: You don't treat disease but you have to treat people - philosophy of
Jikei Hospital. He gave a historical background of Jikei which wasn't translated
well at all.
1) What kind of self-care activities do you engage in your self to Prof. Yuen.
My self-care is my practice. Trained as a chaplain at Thomas Jefferson University
in Philadelphia. She chose the 4 brahamvihara prayer as the principal Buddhist
prayer for the hospital so she also uses the 4 BVs for herself like Ven Bhodananda.
Need to shift gears between analytical and diagnostic methods but then give
way to spaciousness and presence. AT 27:41
2) There is a difference between religious care and spiritual or contemplative
care, so do you feel any contradiction when acting as Christian priest with
Buddhist training to Gustav My not knowing is a great resource in my work
in adapting and finding out what his role best is. There are lots of contradictions
in religion and in religious institutions and teachings. I misunderstood at
the beginning that religious people would die more easily but he found that
to be wrong like when devout Christians ask him why they are sick and dying
since they have been faithful.
3) What was the reason you got involved in this work and what should Japanese
Buddhists do to start getting involved? How do you think monks should be encouraged
to become more socially engaged? Growing up in Colombo he lived near a prison
and every morning saw the prisoners taken to court and being abused and beaten
and the way people were abused by the penal system. He recommends more sila
and samadhi for Japanese Buddhism.
Japanese Commentators:
Dr. Naohito Shimoyama - Department of Palliative Medicine, Jikei University
School of Medicine
Planning to a religious care team with Jin, Yoshimizu and Rev. Tanaka who
passed away a few months ago
In certain areas we are helpless to support patients who have religious needs
and desires so we need their help
He reflected on Elaine's talk and how they themselves as medical people get
down and struggle in their work so self-care and self-compassion is important
Schedule:
13:00 Welcome
13:05 Opening remarks by Rev. Hitoshi Jin, Director of the Rinbutsuken Institute
for Engaged Buddhism
13:15 Three Panelists
14:45 Japanese Commentator
15:00 Break
15:15 Open discussion and questions from the floor
16:45 Closing remarks by Prof. Susumu Shimazono, Director of the Sophia University
Institute of Grief Care
17:00 Finish
Elaine: mindfulness with compassion for holistic health care, Gustav: Zen
meditation and Christianity for a kind of care that is open to all possibilities,
Ven. Bodhi: mindfulness with 4 brahmavihara for rehabilitating the whole person,
not just allowing them to be well-adjusted, to develop social leaders